The Most Important Things Athletes Should Add To Their Surgery Checklist
By the time this goes live, I’ll be recovering from a total knee replacement surgery. About seven years ago, I experienced some pretty significant trauma to my right knee after a ski accident. Turns out, I put my femur through my tibia. I do remember standing up and thinking I’d had a pretty bad sprain. I even told Juliet I probably needed to ski down and end the day, which I did. When I finally realized that I should get some imaging, I was told I should “swim and bike a little” and schedule my knee replacement because it was “pretty bad in there”.
Suffice it to say the joint has had a good run. Last year I deadlifted 605 pounds and ran a Spartan half-marathon. I still have no pain, and a great range of motion, but from a functional standpoint, it was time. Too many things started to come off the table, and quickly. Running, out. Jumping, out. Even mountain biking started to bother me. I knew it was time.
I couldn’t generate the same amount of force with my right knee as my left, and certain positions create a bad feeling in the joint. Coming off a pull-up bar I naturally favor my left leg, and descending stairs with a load is not a fun experience. This summer, I was portaging a big waterfall with my kayak on my shoulders and almost slipped to my death when my knee decided it wasn’t going to tolerate my shenanigans.
To be clear, I wasn’t motivated to have surgery because I was in pain, I was motivated by getting my life back. Though surgery is often viewed through the lens of pain-relief, I was excited to use it as a way to improve my role in work, family, and play.
I’ve probably helped a thousand people manage complex surgeries. I knew that if I wanted an excellent outcome, I’d need a plan.
My first and foremost goal was to manage the surgical insult and its immediate acute effects. Normally we operate within a structure of our own making: community, daily rituals, training, and whatnot. Going under the knife not only limits our ability to move the joint but also breaks us from the communal environment we have built around ourselves. My goal was to manage the surgical insult immediately, so I could heal at the maximal rate humans are capable of, decrease post-surgical swelling and related pain, and be less of a burden to my busy family.
Continuing to move in pain-free ranges of motion, managing swelling, hyper-optimizing lifestyle factors like nutrition and sleep, and continuing to train with your community is essential. This is the plan we use with our clients, and this is what I’ll continue to do to optimize the healing process.
For me, surgery doesn’t begin on the day you walk into the hospital. The process begins long before that. In short, control what you can control and set yourself up for success. Here is my surgery checklist for athletes:
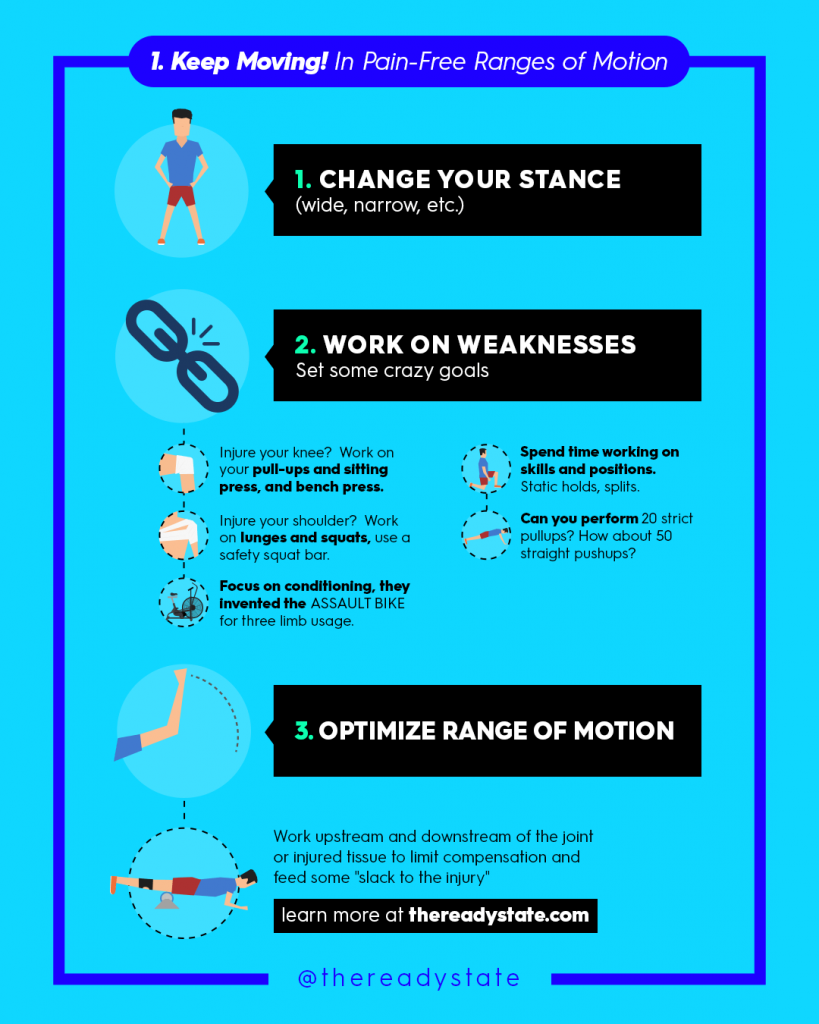
Continue To Move In Pain-Free Ranges Of Motion
When we experience orthopedic trauma that requires surgeries, it’s easy to forget that there is a real benefit to continuing to move. As Coach Dan John says, “do what you can, where you are, with what you have.”
Whatever the limitations of your injured joint, keep moving in as many pain-free ranges as possible.
- Change your Stance: Instead of compensating for the joint by favoring one leg, widen or narrow your stand til’ you find pain free stability
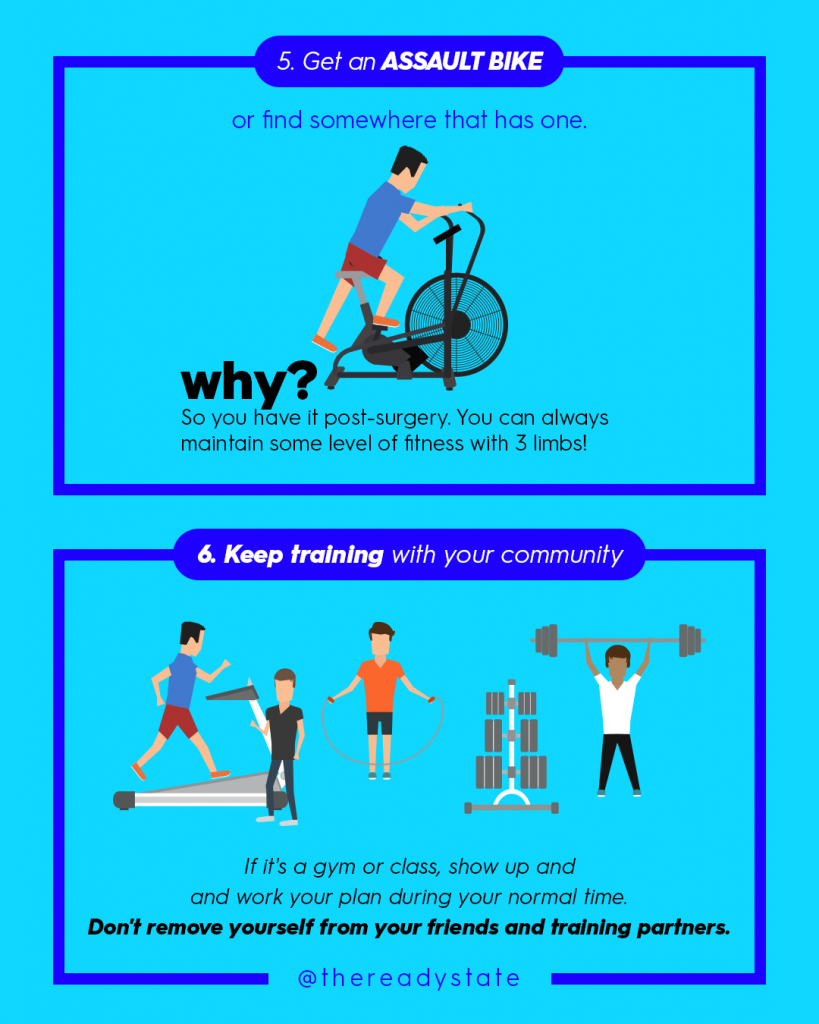
- Work on your weaknesses: This is a great time to shore up your weaknesses. Set goals for pain-free movements. Work on your pull-ups or bench press, and focus on conditioning! Get on the assault bike with 3 limb-usage!
- Optimize your range of motion. Continue doing your Ready State daily mobility work. Remember if it feels sketchy, it is sketchy. Address mobility restrictions throughout your body. Work upstream and downstream of the joint to limit compensation and feed some “slack” to the injury. Our goal is blood flow and healthy tissues. Keep the range of motion you still have.
Start these habits pre-emptively so you can build a structure you can more easily modify and return to post-op, while also preparing your body pre-op.
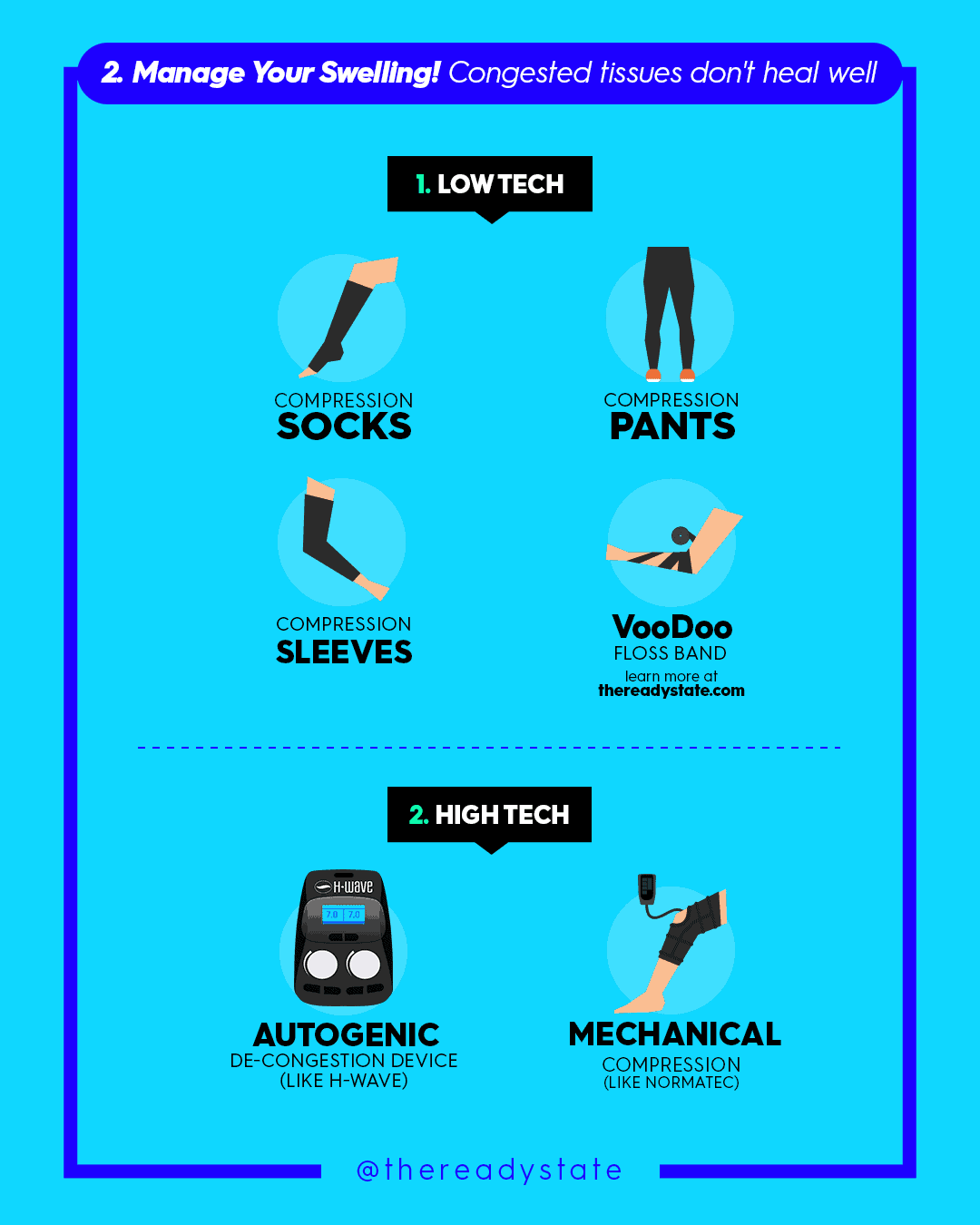
Manage Your Swelling
My main prerogative is to get ahead of the swelling and to do that, we want to create activity and motion inside the tissues. The good news is that the same protocols we use to adapt to strenuous training can be applied to clear congestion after surgery.
How do we do this? We have low-tech and high-tech options.
Low Tech: Compression
Compression is how we can mechanically decongest swollen tissues. Even compressing your opposite limb can have a beneficial effect through vascular changes caused by chemical signaling.
Voodoo floss, compression socks, pants, and sleeves prevent congestion. Remember, congested tissues don’t heal as fast they might otherwise.
Don’t use this gear while the joint is still numb or over your incisions, but absolutely utilize compression before surgery and, when you can, after.
High Tech: Autogenic, Normatech & BFR
Autogenic: Autogenic devices like the H-Wave that I’ll be using stimulate muscle with an electrical frequency. These are not like TENS devices that are superficial, but actually create muscle contraction. We can think of this as movement without motion.
Your lymphatic system is the sewage system of your body. It’s connected directly to your movement system (convenient). Swelling is a vital part of your healing process. We need to not limit healing (swelling) but rather the stagnation in those lymphatic tissues. Injury, strain, and surgical trauma make it hard to move enough to adequately decongest.
Normatec Boots: The NormaTec Boots create mechanical compression and increase blood flow. I alternate between the boots and my H-Wave.
Bloodflow Restriction Therapy: One of the most well-researched tactics for physical rehab is blood flow restriction therapy (“BFR”). This has been around forever and is often used for muscle gain, but in the case of an operation can be used to effectively promote healing. There is a ton of research supporting BFR for analgesia as well as improved blood flow. The research also supports big kicks in the hormones that help rebuild tissues after trauma.
To bring this all together definitely check out my video on Instagram Surgery Series Part 1: Short Term Goals.
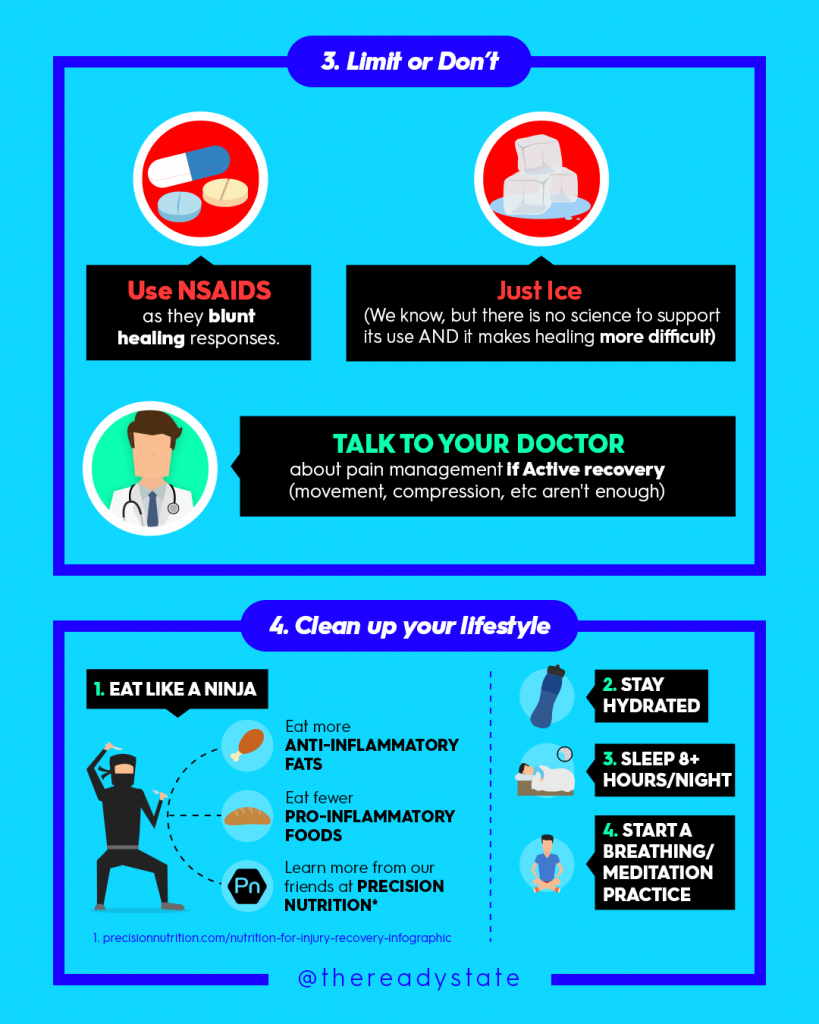
Get Your Lifestyle Optimized

Avoid icing and NSAIDs (non-steroidal anti-inflammatories.) NSAIDs blunt the healing process and icing doesn’t have good science supporting it. On top this, icing may limit your ability to evacuate swelling which may make healing more difficult. I know that’s probably triggering to hear from some folks, but if you want the full explanation go read my article: You’ve Got To Stop Icing.
Beyond this, up to your protein intake and sleep like it’s your job. I’ll be consuming 170 to 200g of protein daily to support recovery as I go through the healing process. I want to make sure I have everything my body needs for rapid tissue repair.
Of course, I’ll also be prioritizing quality. If there was ever a time for it, this is it. Go check out our friends at Precision Nutrition if you need help in this arena.
Finally, with regard to sleep, I’ll definitely be napping and aiming for at least 9 hours of sleep per 24 hours cycle.
As my friend Dr. Kirk Parsley says, 8 hours is the base. Less than that and you’re turning on the stressed brain, and if you are active, injured, or recovering then 9+ hours should be a priority.
Keep Training With Your Community
Mentioned this in the beginning but it bears repeating. You have a whole environment built around you that your mind treats as “safe.” Don’t get ostracized from it by surgery. As soon as you can, get back to your training community. Even if you can’t do the group WODs yet, it’s better to show up and modify than sit at home.
We are communal beings. Tribal beings. It’s hard enough to find connections in the modern world and your primate brain knows it. If it sees you isolating at the same time you have an injury, it’s gonna feel abandoned and up those stress responses.
Not sure what to do while you’re with your gym community? Like I said earlier, you can still use an assault bike with only 3 limbs. Focus on pain-free ranges of motion, keep your conditioning up, and stay in your tribe.
And that’s it for now! As I said, I’ve got a great video covering most of this stuff over on IG labeled Surgery Series Part 1: Short Term Goals. I also have Part 2: Set Up Your Environment that will coincide with another article like this.
DOWNLOAD THE PRE-SURGERY PDF















Thanks for sharing (even more of) your experience, wisdom and guidance, Kelly. My ortho recently suggested I plan for a right knee replacement in a few years (where “few” wasn’t the number I had in mind…) X-Rays were telling. I have worked to compensate, and your guidance above will add to my mitigation and planning for what could be inevitable, too. I’ll watch your IG video, next.
OMG, sorry for you Dr Starrett but I am so happy to see this info! I am 2 weeks out from TKR on first knee, second this spring. I am in the same situation of WHY I am doing it, not from pain, but such decreased ROM that I have finally had enough. I know you have documented a lot on IG, but is there another way to view the videos on the dashboard as a Ready State member?
Hi Kelly!
I know your pain. I had both knees replaced in 2003, they were done about about a year apart. The first one was hard, the second one was not. I guess you know what expect. I am a retired physical therapist and at the time of my surgeries I was still working. All of the info you outlined was really not available at that time. The use of ice was very common and activity was really reduced because of post surgical advice from my doctors. Of course i didn’t take that advice because my practice was based on functional exercise return to sports. It went well despite some warnings to not work so hard. The truth is that activity made both knees feel better, reduced swelling and helped me return to normal activity levels. Thanks for the great outline in you post and if anyone is having a knee done follow these ideas for a great outcome.
Tim Daley PT