FROZEN SHOULDER: What It Is and How To Tackle It
Let’s start with this. Our shoulders are designed to be the most versatile and mobile joints. We use them to perform a plethora of things from functional tasks such as feeding ourselves to high-level activities such as throwing a ball 100 mph or handstand walking our way into the Guinness Book of World Records. When we lose the ability to access the full capacity of this amazing joint due to frozen shoulder, it sucks! Although there are several unknowns about how or why this develops, it can be a physically and emotionally draining experience.
But don’t worry because we’ve come up with a guide to tackle it head-on.
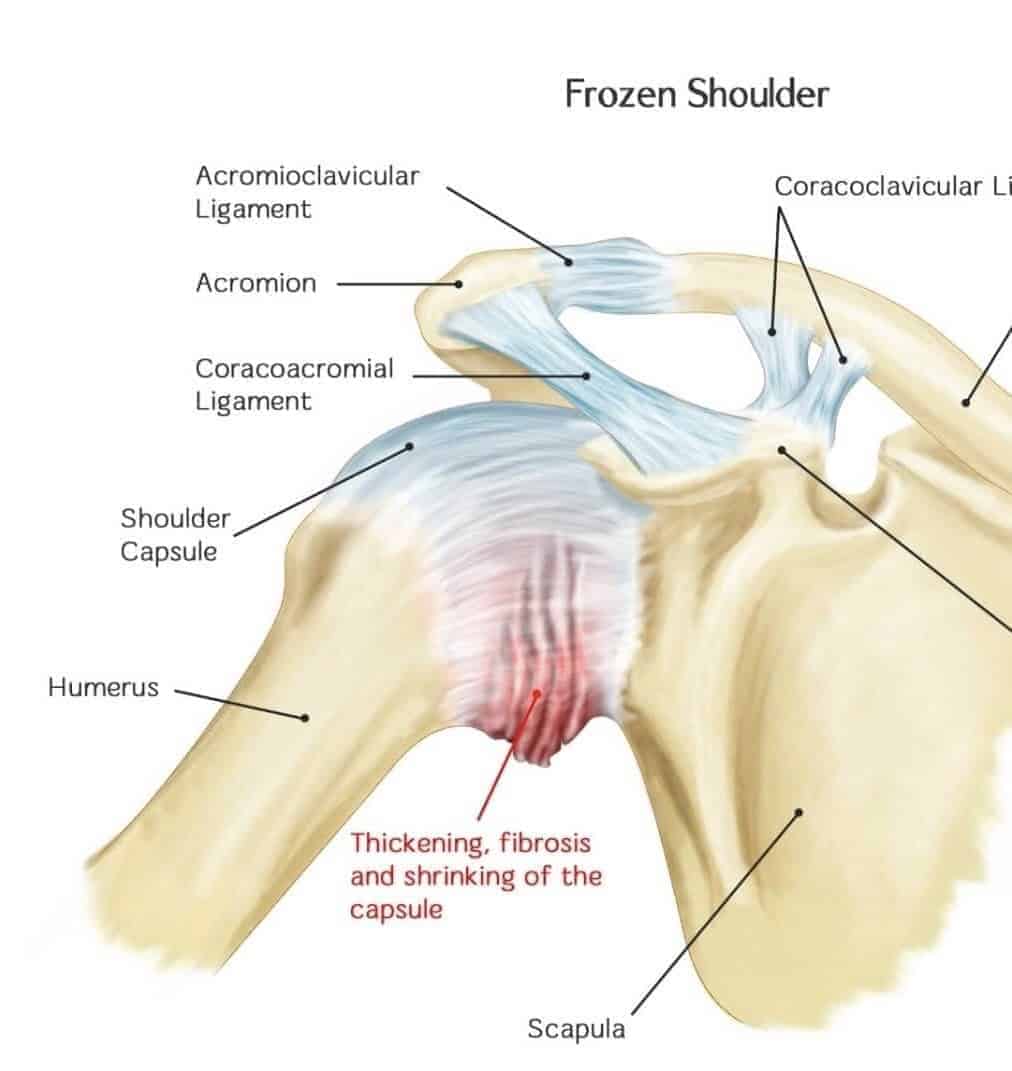
What is Frozen Shoulder?
Frozen shoulder (aka – Adhesive Capsulitis) is the stiffening of the capsule or casing that surrounds the ball, socket, and the muscles of the shoulder joint. The capsule, which is a blend of fibrous tissue, acts as a backup to keep the ball within the socket when the muscles of the shoulder can’t. This stiffening of the capsule results in legitimate restrictions in the range of motion of the shoulder, especially in the direction of external rotation and abduction, and it can be painful.
Let’s think about it this way. Imagine that the capsule is your favorite wool sweater and that it accidentally gets thrown into the dryer. That sweater shrinks and you now are the proud owner of a belly shirt. No longer does it fit you the right way, but it also restricts your ability to freely move. You end up with a diminished ability to access the full capacity of the joint. Motion AND joint mechanics are affected due to this shrinking of the capsule. In other words, the shoulder is stiff AF.

Frozen Shoulder is generally broken down into these 3 phases:
- Freezing Phase – this is the painful phase and it usually lasts 3-6 months
- Frozen Phase – pain subsides, stiffness gets worse and can take place for 4-12 months
- Thawing Phase – regain in motion that can take 6 months and up to 2 years to resolve
Muscle strains can cause shoulder pain/muscle guarding and can make the diagnosis more complex, so what separates a shoulder that presents with a muscular injury FROM a frozen shoulder?
The amount of active range of motion (AROM) versus the amount of passive range of motion (PROM). We tend to see greater amounts of PROM versus AROM when the main movers (muscles) are relaxed. This enables full access to our ligaments/capsule at the end ranges of our joint mechanics.
The hallmark signs seen in someone with frozen shoulder is that there are equal amounts of AROM and PROM, which indicates that there is a restriction of the capsule because we aren’t able to move the shoulder any farther even though the muscles are relaxed. This results in the loss of joint mechanics and joint congruency which ultimately affect stability, performance and in this case, function.
Frozen shoulder can either come on without any incident or can develop as the result of compensatory habits or movement avoidance behaviors due to nagging pain. It is proposed that there is an imbalance between aggressive fibrosis and a loss of normal collagenous remodeling, which can lead to stiffening of the capsule and ligamentous structures.[1]
Couple that with the daily habits of modern living and what we have is a recipe that allows us to fall deeper into the hole and creates an opportunity for our tissues to lose their identity.
Katy Bowman, the author of Move Your DNA, describes a phenomenon known as mechanotransduction, which suggests that mechanical stress/input is necessary to dictate how our cells express themselves. In other words, if we aren’t moving and loading our tissues and joints to the end ranges of our physiological limits on the regular, they de-evolve.

There’s a common belief that frozen shoulder will resolve on its own. Based on recent research this is untrue. Individuals with untreated frozen shoulders (meaning do nothing) still presented with persistent limitations lasting 4 years after onset.
So now that we have a better understanding of what frozen shoulder is, the question is, what can you do about it?
Take a Crack at Fixing Yourself
Let me preface this by saying that I’m a physio. I confess! Early in my career I would have said that the best way to treat a frozen shoulder, is to seek the help of a physio or chiro for manual therapy. What I learned as I treated more and more patients, is that it quickly became a test of who could withstand the most torture, uh I mean, skilled hands on intervention. Now, if you’re into that sort of thing, rock on. But the last thing that I wanted was for my patients to associate their experience and time with me as an unsafe and painful one. I also didn’t want them to feel that their outcome was dependent or tied to a need to work with a professional.
Pain that is commonly associated with frozen shoulder is real. The advantage of taking a crack at it yourself offers you an internal loci of control. I repeat, taking a crack at it yourself offers you an internal loci of control.
If you aren’t experiencing what we deem as medical Red Flags (such as unexplained weight loss, night sweats, fever, vomiting, etc ..), the Pain pathway here at the Ready State has a ton of interventions to move the needle forward.
Modulate Your Relationship With Pain
Breathe!
Protective muscle guarding is thought to be a huge limiting factor in making authentic gains in ROM in those with frozen shoulder. And being in constant pain or demonstrating fear-avoidance behaviors can place an emotional toll by affecting sleep and mood. Begin by adding some non-threatening input with Box Breathing to tap into the parasympathetic you. You may have heard Kelly or Gray Cook say that if you can’t breathe in a position, you don’t own that position. So start to take the handbrake off your motion limits by incorporating a breathing practice into your routine.
De-Sensitize
Begin to restore the normal sliding surfaces, tissue environment and the relationship of the joints. Typically, we see missing components in the Front Rack Archetype. If you are uncertain of what the benchmarks are in this archetype, you can find it here.
But what we’ve also found is that improving the neighborhood can yield positive global changes. Focus on areas not just in the shoulder, but also in areas such as the scapula, neck and thoracic spine.
In the meantime, here are some good places for you to start to tackle some common limits seen in frozen shoulder.
Be Consistent
Consistency is more important than intensity, especially in the early stages of frozen shoulder. Carve out 10-15 minutes daily with a mindset of purpose and intent. Create a checklist or keep a journal to measure your progress. Check out this neat google calendar spreadsheet from the How To Get READY: 3 Ways to Achieve Your Ready State blog.
Again, going back to the principle of mechanotransduction. Restoring the integrity, composition and function of the soft tissues of the said shoulder joint will happen if they are stressed often and appropriately.
Adaptation takes time.
Stop me if you’ve heard this one before.
“Tissues are like obedient dogs.”
~ Kelly quoting his pediatric PT professor
But I bet you haven’t heard this one.
“If you give only 80 percent leadership, your dog will give you 80 percent following. And the other 20 percent of the time he will run the show. If you give your dog any opportunity for him to lead you, he will take it.”
~ Cesar Millan
Be a calm and assertive pack leader!
If It Feels Sketchy, Then It Is Sketchy
Lastly, if you feel like you’ve been hammering away and feel like you’re not getting anywhere, it may be time to reach out to your local healthcare professional (physio, chiro, MD). And if you’re a bit overwhelmed and not sure where or how to start? Check out our List of TRS Providers.

















TRS Virtual Mobility Coach
Guided mobilization videos customized for your body and lifestyle.
FREE 7-Day Trial